Tomographic reflection combines visual and ultrasound images
Andrew Wilson,Editor,[email protected]
Invasive surgical procedures such as tissue biopsy often are guided by ultrasound systems, allowing doctors to plan the point of surgical entry and maneuvers around critical muscles and organs to reach the point of interest with minimal trauma to the patient. In performing invasive procedures, physicians must look away from the patient to view the guiding ultrasound images. Such indirect hand-eye coordination systems can limit the physician's ability to easily find specific areas of interest without damaging the surrounding critical structures.
To overcome this limitation, George Stetten, assistant professor in the department of bioengineering at the University of Pittsburgh and the Carnegie Mellon Robotics Institute (Pittsburgh, PA; www.stetten.com/george/rttr/) has developed a method that combines visual images with ultrasound images. In this process, called tomographic reflection, the visual outer surface image of the patient is merged with a simultaneous ultrasound scan of the patient's interior. This resultant image allows the physician to visualize the skin and underlying tissues as if they were translucent. As a result, the physician no longer has to look away from the patient to see associated ultrasound images because they now appear merged with the outer skin of the patient.
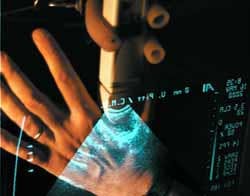
Stetten developed both an immobile stationary prototype system and a portable hand-held device that he calls the Sonic Flashlight (see figure). In the development of this prototype, he had to accurately register the captured ultrasound slice with the visual image. To do so, the Sonic Flashlight uses a 12 x 9-in. half-silvered mirror that bisects the angle between the ultrasound slice and a flat-panel monitor. Points in the ultrasound slice and their corresponding locations on the monitor are equidistant from the half-silvered mirror along a line perpendicular to the mirror distance. And, because the angle of incidence equals the angle of reflectance, the surgeon sees each point in the reflection at its corresponding physical location.
After images are captured with an ultrasound machine from Pie Medical (Indianapolis, IN), they are digitized using a PC-based video-capture board from Matrox (Dorval, Quebec, Canada) and displayed on a flat-panel monitor made by Pixtech (Santa Clara, CA). According to Stetten, these devices can capture and display images at 30 frames/s.
To demonstrate the method, a human hand was imaged with the ultrasound transducer pressed against the soft tissue between the thumb and index finger (see figure). The external surfaces of the hand are collocated with other structures within the ultrasound image. "Unfortunately," says Stetten, "the photograph cannot convey the strong sense derived from stereoscopic vision that the reflected image is located within the hand. This sense is intensified with head motion because the image remains properly aligned from different viewpoints. To one experiencing the technique firsthand, ultrasound targets within the hand are clearly accessible to biopsy or incision."